As TEC rapidly evolves beyond its traditional analogue alarm-focussed roots, the enabling factors required to help people adopt and benefit from TEC are also changing. With the transition to digital infrastructure and the rise of smart technologies, we are moving into a more dynamic, data-driven environment. Today, proactive products and services aim to prevent decline and actively support individuals, going beyond just providing a safety net. However, this increased capability adds complexity and alters the enabling factors required for users to fully access and benefit from this technology.
So, what are the key enablers of Technology-Enabled Care in this evolving landscape?
Alarm-based Telecare – From Connectivity to Continuity
Traditional alarm-based telecare allows individuals to request assistance via a wireless pendant or a button on their alarm hub, or automatically through sensors such as smoke or fall detectors. Legacy analogue telecare alarms connect to a monitoring service using a copper landline telephone (PSTN) connection, which requires a nearby phone and power socket. When a landline service is unavailable at the property, a mobile connection can be used as an alternative. These systems are dependable, with backup batteries ensuring continuous service during power outages.
Digital telecare hubs connect via a 4G mobile network and/or fixed-line broadband, with a dual approach recommended for enhanced resilience. They are also equipped with backup batteries that can last several days. For fixed-line broadband connections, an additional battery backup is required for both the router and, if present, the Optical Network Terminal (ONT), which is necessary for Fibre-To-The-Home (FTTH) services. Additionally, digital hubs must now support digital voice channels using VoIP and 4G Voice (VoLTE), as 2G networks are being phased out.
Therefore, the key technical enablers for digital telecare include:
- A digital alarm hub with Ethernet and 4G (VoLTE) connectivity
- Reliable 4G mobile coverage across multiple national and core network operators
- Dependable broadband with backup power for at least one hour, preferably more
Additionally, individuals often need to appoint ‘keyholders’ to respond in emergencies, especially if formal services are unavailable. Using key safes to enable easy property access if the resident cannot answer the door is also considered an essential part of a telecare service.
Thus, for basic services, if these conditions are satisfied and the user can activate their alarm pendant, a conventional telecare service becomes a straightforward component of a care plan.
The Transition from Alarms to Proactive Support
Proactive telecare is increasingly recognised as a valuable tool in the support and care sector. It uses data from sensors to monitor activity, health parameters, and environmental conditions, observing notable changes in patterns that may indicate a need for intervention. This type of telecare is passive, meaning that the individual usually does not need to request help; the system operates automatically and can facilitate preventative services that intervene before an emergency arises.
The nature of this intervention might initially be directly aimed at the individual, perhaps through a prompt (e.g. to remind them to close the front door or that they have a health appointment in the morning). Alternatively, it could involve notifying a family member or a monitoring service of specific situations that might require further investigation, such as a noticeable change in the individual’s activity levels or if they have not had their usual morning cup of tea.
Increasingly, systems are emerging that use consumer devices, such as smart speakers with voice assistants (like Alexa) or touchscreen controls, for managing smart technology in homes, providing information and support and conducting video calls with family members. Some make use of wearable devices that monitor activities, health parameters, and location, and which can detect falls or enable the user to easily contact a responder in an emergency.
Another crucial factor is the interoperability of both home and wearable technology, as well as backend systems that facilitate data pooling. This represents a significant shift from legacy Alarm Receiving Centres, enabling more advanced data analysis and the use of artificial intelligence (AI) via machine learning. The combination of data integration and AI allows the delivery of useful, context-aware, and timely responses to evolving situations.
Moving from Hardware to Software (Apps)
Another significant trend involves the use of apps on individuals’ smartphones or tablets, as well as those of their carers, to deliver applications that were once provided using a specialist and dedicated piece of hardware. This offers several benefits, including a potentially more cost-effective solution and the advantage that users familiar with their smartphones require less support. Smartphones feature multiple sensors, GPS geolocation, and reliable connectivity, allowing for seamless integration with other digital devices and platforms. However, a drawback is that if the smartphone runs out of battery or is lost, several support options are lost simultaneously.
A wide variety of apps are available, some aimed at general use but capable of supporting independent living, while others are specifically developed for the care and independent living sector. It is essential to recognise that the quality of these apps varies significantly, and this should be assessed before relying on one to support an individual. It is also true that sometimes a more specialised hardware product, assistive device, or system might be the best solution in certain situations.
Examples of the types of support available through apps include:
- General-use applications such as staying in touch with family and friends or wider social networks, performing online shopping and banking, and for entertainment like watching television, films, or listening to music or the radio.
- Supporting people with visual impairments in identifying or describing the contents of a room, reading a sign or document or recognising the colour of an object.
- Helping an individual to plan the tasks they need to undertake in their day, e.g. to get to work on time.
- Providing video tutorials to individuals to assist them with everyday tasks and to monitor their use of these to determine if they are now proficient in each task.
- Monitoring health parameters and managing prescriptions.
- Providing opportunities for leisure activities such as video games and educational or therapeutic interventions via virtual or augmented reality headsets.
Moving Beyond Passive ‘Service Users’
With telecare, a person contacts or is referred to a service provider who supplies technology-based services, preferably based on an assessment of their needs or as an electronic safety net where the needs are less clear. This is installed in the home by a professional, who tests its proper functioning and demonstrates how to use it before leaving. The individual then receives a 24/7 monitoring service to respond to any alarms that may be raised. Individuals who subscribe to a telecare service are often referred to as ‘service users.’
Increasingly, products and apps can be self-installed and even self-purchased in an ad hoc manner, especially with mainstream consumer products or apps. These often come with easy access to online videos to guide self-installation and operation. While many individuals will still need a comprehensive service to help them identify, select, install, and monitor care technology products and services, some will opt to do it themselves, with the help of family or friends, or follow a hybrid approach.
As the range of care technology expands beyond alarm provision, technology can be used to support individuals in their everyday lives, not just when problems arise. To accommodate this shift, the roles of service providers and monitoring services will need to evolve from a prescriptive and reactive model to a more advisory, supportive, and proactive one. Such a change will not be trivial and may not be achievable for all organisations.
Building Trust
As care becomes increasingly digitised and reliant on the collection of personal data that has the potential to trigger interventions, we must ensure that people are supported by technology on their own terms. People must be supported throughout their TEC journey, from identifying their goals and wishes to solution discovery, onboarding, and ongoing support. They must be empowered to use TEC purposefully and confidently, knowing that help is on hand if needed. Compliance with agreed industry standards and best practices is essential. Issues of data security and privacy, informed consent and other ethical concerns, such as who benefits the most from its use, must be carefully considered. Sharing data and insights with third parties, including family members, should only happen if it is explicitly agreed upon with the individual.
Proactive telecare is still viewed as a risk by some due to the significant service changes required and the uncertainty associated with selecting an appropriate technology and/or service provider partner. Within the sector itself, a strong evidence base for the effectiveness of TEC approaches would help build trust by enabling the positive outcomes and benefits for all stakeholders to be documented and independently verified. This would help service commissioners to develop and invest in new service models based on proactive, technology-enabled care services.
Finally, the longevity or commercial sustainability of suppliers must be considered alongside mitigation strategies in case they fail, exit the market, or transfer their assets to other providers.
Digital TEC Enablers
In summary, to achieve positive outcomes using technology-enabled care, individuals require a combination of practical, technological, and systemic enablers. This involves rethinking enablers not merely as ‘removing barriers’ but as fostering relationships between individuals, technology, and care systems. These issues are outlined according to four main areas, as shown in Figure 1, and are explored further below.
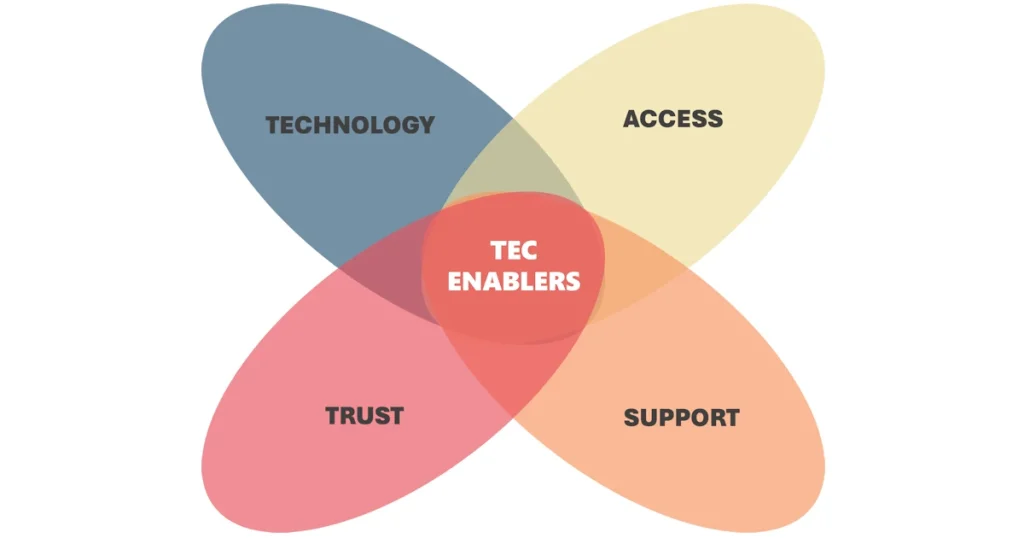
Technology
The primary enabler is the availability and selection of appropriate technology, and the infrastructure that needs to be in place to support its use:
- A diverse, flexible range of easy-to-use, reliable, and aesthetically pleasing technology solutions tailored to individual needs.
- Interoperable systems that work across multiple suppliers, enhancing resilience and enabling intelligent, context-aware services.
- Dependable home connectivity with backup options to maintain service during outages, along with dependable community connectivity to support people outside their homes.
Access
It is essential that those who stand to benefit the most from technology can easily access it. This encompasses a wide range of factors:
- Raise awareness among the public, service providers, and commissioners about technology-based solutions that support independence and person-centred care.
- Ensure individuals, families, and professionals can access independent guidance on suitable technologies, their costs, and how to obtain them.
- Professionals should be trained to navigate the wide range of technologies available and recommend the most suitable ones to individuals.
- Promote a culture of innovation and the adoption of new, value-for-money technologies, balancing specialist and consumer options based on assessed needs.
- Support digital literacy so users and their families feel confident operating and maintaining technological products.
- Develop strategic policies and invest in expanding a successful technology-enabled care sector for an ageing population.
Support
Ongoing support must be available to help ensure that any issues or problems are resolved promptly, and to reassure people that they are not alone:
- Provide accessible onboarding and training for users and their support networks.
- Ensure ongoing support through both informal carers and formal services like 24/7 helpdesks and emergency assistance.
- Offer a formal response service for non-emergency situations lacking informal responders.
- Include preventative support, not just crisis intervention.
Trust
People should be highly motivated and inspired to adopt a solution, based on a clear understanding of its benefits:
- Build clear evidence of a technology’s benefits to encourage adoption.
- Ensure products are dependable, with robust data protection and informed consent mechanisms in place.
- Be transparent about what data is collected, how it is used, who has access to it, and for what purposes.
- Follow sector standards for interoperability and transparency about device support and updates.
Conclusions
The effective use of care technology to support people to live well depends on a holistic approach, where onboarding, ongoing support, and both preventive and responsive services are seamlessly integrated. The key is making onboarding processes accessible not only to users but also to their support networks, ensuring that everyone is aware of, prepared for, and confident in using the technology. Ongoing support, provided by both informal carers and formal services, offers the continuity and reassurance that users need. Additionally, establishing a formal response for non-emergency situations ensures that no one is left without help.
It is essential to look beyond crisis management and promote preventative support, empowering individuals before challenges escalate. Building trust stands at the heart of adoption: both users and service providers must be motivated and see the benefits of these solutions. This trust is based on clear evidence of effectiveness, strong protections for data and consent, and dependable products that address real needs while following industry standards for interoperability and providing transparency about product lifespans.
To unlock the full potential of technology-enabled care, it is essential to foster a culture of innovation among telecare commissioners and providers, moving beyond reactive models to embrace person-centred, preventative support. This transition requires encouraging creative thinking, accepting manageable risks, promoting collaboration, and investing in workforce development to enhance digital confidence and flexibility. By championing openness to change and empowering staff at all levels, telecare services can evolve into a more proactive and supportive service that genuinely meets the needs and aspirations of the people they support.
In summary, the successful adoption and sustained use of digital care technologies depends on reliable, user-focused, and cost-effective solutions, strategic investment, service redesign, accessible training, comprehensive support, clear benefits, and a focus on user safety and trust. Together, these factors will enable the future of technology-enabled care.
