For decades, alarm-based telecare systems, comprising pendant alarms, pull cords, and passive sensors connected to a dispersed alarm unit, have been the backbone of Technology-Enabled Care (TEC) services worldwide. These services have provided a vital safety net for thousands of people living at home, offering them quick and easy access to support and assistance in an emergency.
However, in today’s care landscape, where the goals are prevention, personalisation, and outcomes-based commissioning, alarm-driven models are deficient. This is especially true when we consider the widespread availability of relatively affordable mainstream consumer technologies that help everyone manage their daily lives. Demonstrating that all technology, in a way, can be considered assistive technology.
At T-Cubed, we believe it’s time to rethink the role of care technology – not merely as a safety net, but as an enabler of supported and independent living, where technology does more than act as insurance when bad things happen, and enables individuals to live their best lives.
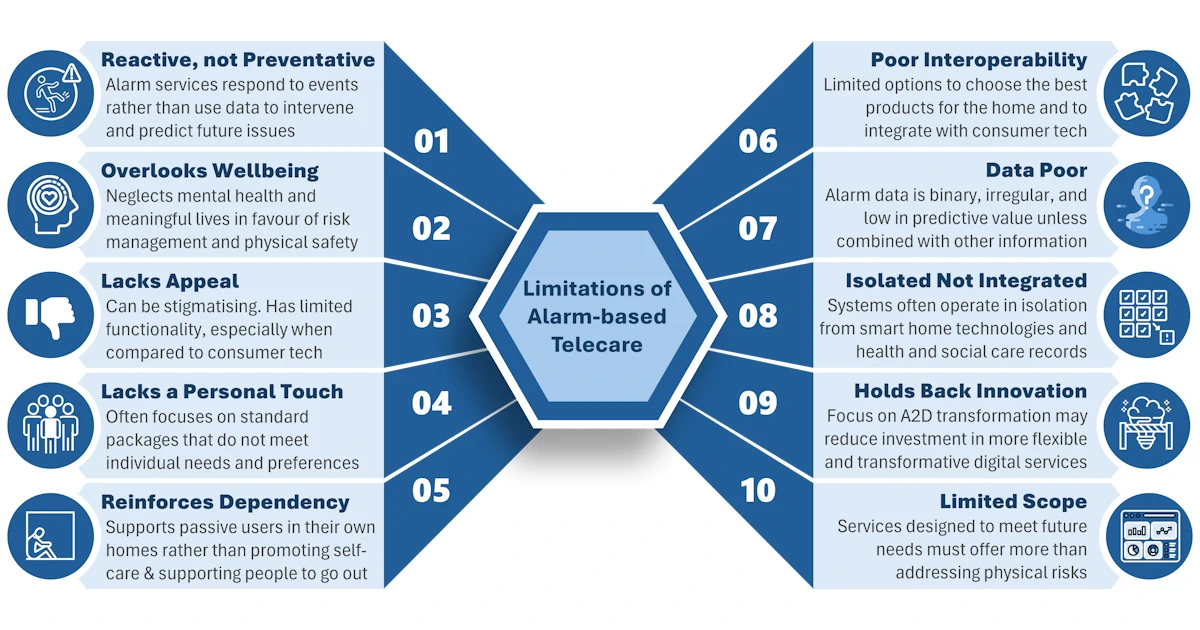
In this brief article, we explore the limitations of the traditional alarm-based model, which are summarised in Figure 1 above.
1.It’s Reactive, Not Preventative
Alarm-based services are designed to respond to crises, but they do little to help avoid them. A fall has already happened, a fire has already started, and a person may already be in distress. Furthermore, a person could be experiencing declining physical or cognitive health without any alarms being triggered… individuals who do not set off an alert are often invisible to the system.
Modern data-driven care technologies offer a better alternative, providing passive monitoring, trend analysis, and early warnings that can prompt proactive interventions. This can reduce harm and pressure on services, enabling earlier intervention to achieve better outcomes for individuals and their families.
2. It Overlooks the Broader Perspective of Wellbeing
Traditional telecare focuses on managing risks and physical safety, supporting the lower levels of Maslow’s hierarchy of needs. However, it doesn’t support the broader dimensions of wellbeing that matter just as much and can make life worth living, such as mental health, social connection, confidence, and purpose.
If technology is to help people live fulfilling lives, not just safe ones, then it must do more than just raise alarms after the event.
3. It Lacks Appeal to Many Users
Pendants and pull cords have a certain stigma attached to their use – a so-called ‘badge of dependence’. Many users, especially working-age adults or those with hidden disabilities, don’t see themselves as needing these products or services. This is particularly true for people who regularly use smartphones or other smart devices in their homes.
A modern technology offer should be inclusive by design: discreet, dignified, unobtrusive, contemporary and able to serve a diverse population on their terms.
4. It Doesn’t Personalise Support
Alarm-based services are often based on standardised packages, regardless of age, goals, or lifestyle. But people don’t fit neatly into risk categories, and tick-box approaches are not the answer. Even when packages are well-matched to an individual’s needs, they still only provide a reactive ‘insurance’ against bad things happening.
Commissioning for personalisation means enabling users to choose the tools that work for them, whether that’s self-managed apps, voice-enabled routines, smart home devices, wearables, or connected community platforms.
5. It Reinforces Dependency
Ironically, services designed to preserve independence can sometimes have the opposite effect. Alarm-based models often create passive users, waiting to be helped. Traditional telecare is also based around the home, without support for individuals when they are outside in their communities.
Reactive alarm systems do not provide users or carers with access to meaningful data, so they cannot obtain personal insights such as changes in sleep patterns, physiological measurements, or activity levels. The opportunity to make informed data-led adjustments to improve health and wellbeing is lacking.
Modern care technology should enable people to manage their own needs, stay active in their communities, and feel in control of their own lives.
6. Interoperability is Poor
Although progress has been made with standardised alarm protocols between equipment in the home and alarm monitoring centres, there has been no advancement in opening up the device environment within the home to enable a mix-and-match, best-of-breed approach. There is also limited scope for integration with smart home systems that could provide additional sensors and allow control of the local environment.
This can lead to missed opportunities to engage with the individual or their home to support their independence, prevent future issues, or can result in unnecessary duplication of technology.
7. It Doesn’t Make the Best Use of Data
Alarm-based telecare relies on reactive data collected after an incident or alarm has been triggered. Such data is binary, irregular, and event-driven, often lacking context. Furthermore, variations in how call reasons and outcomes are documented hinder the potential for meaningful data analysis.
There is often no information collected about why the event occurred, how the user was feeling beforehand, or what patterns may have contributed to it. This makes it very difficult to understand someone’s baseline wellbeing, identify trends over time, or provide proactive context-aware or preventive support.
8. It Doesn’t Integrate with the Wider Care Ecosystem
Too often, traditional telecare operates in isolation, unlinked to GP or social care records, social prescribing, or community support. Furthermore, the limitations of the available data and the lack of agreed-upon coding standards complicate or render data sharing impossible.
That’s a missed opportunity. Today’s care challenges demand connected systems that share data, coordinate care, and provide a single view of the individual across health, housing and social care.
9. It Holds Back Innovation
As long as commissioning stays focused on alarm models, transformation stalls. Commissioners need to unlock investment in flexible, digital-first services that support prevention, self-care, and population-level intelligence. Numerous examples of new and innovative products that can meet these needs exist, and many more enter the market each year.
The future of TEC shouldn’t just be about replacing analogue alarms with digital ones. It’s about designing services that work for the whole person and the system around them.
10. Its Scope is Limited
Traditional alarm-based telecare remains a vital part of any care technology approach and will continue to deliver a valuable service to a limited number of specific, vulnerable individuals. However, it is no longer enough by itself to meet the evolving needs and expectations of individuals, commissioners, or integrated care systems. It can provide a safety net, but, as things stand, it does not offer a platform on which to build intelligent, always-available, context-aware applications that can support personalised and preventive services.
Commissioners and service providers must now move toward care technology models that are:
- Flexible and personalised
- Data-rich and insight-driven
- Designed around wellbeing, not just risk
- Integrated with wider systems
What This Means
Technology-enabled care needs to evolve from relying on reactive alarm-based monitoring to a new, data-rich model with continuous monitoring that supports context-aware applications, data-driven insights that facilitate self-care, and triggers interventions before emergencies occur. This requires the use of interoperable systems that work with integrated monitoring and care platforms, featuring person-centred dashboards and analytics.
If you’re responsible for shaping TEC services in your area, now is the time to transition from a purely reactive approach to a data-driven one and switch from activity-based contracts to outcomes-led commissioning.
That means:
- Prioritising prevention and early intervention
- Commissioning solutions that support wellbeing, not just emergency response
- Selecting platforms that prioritise interoperability and are guided by user needs
- Embracing innovation that enables community-based, independent living
At T-Cubed, we collaborate with commissioners and service providers to help them evaluate and develop their services, ensuring they are personalised and prepared for the future.
